Aspergillosis
What is Aspergillosis?
Most fungi reproduce via sexual or asexual spores. These structures, although tiny, are equipped to withstand many difficult environments and carry all that is required for a new fungal life to begin. However, the chances of every spore to land in a hospitable environment and to successfully germinate are very low. Therefore, fungi rely on producing and releasing copious amounts of spores to increase the chances of successful reproduction. Studies have shown that most fungi release chances of successful reproduction. Studies have shown that fungi are capable of releasing hundreds of millions of these tiny spores daily when sporulating (1,2).
Healthy humans take in these spores without any problems because our immune systems have evolved over millions of years to constantly find, restrict and eliminate these structures from our bodies. Some fungi are animal pathogens, but most fungi and their spores are harmless to healthy human beings. Our neutrophils (a type of white blood cells) are fully capable to deal with any fungal spores that make it to our lungs, upon inhalation. Most spores, though, do not reach our lungs and end up in the upper parts of the respiratory tract (3).
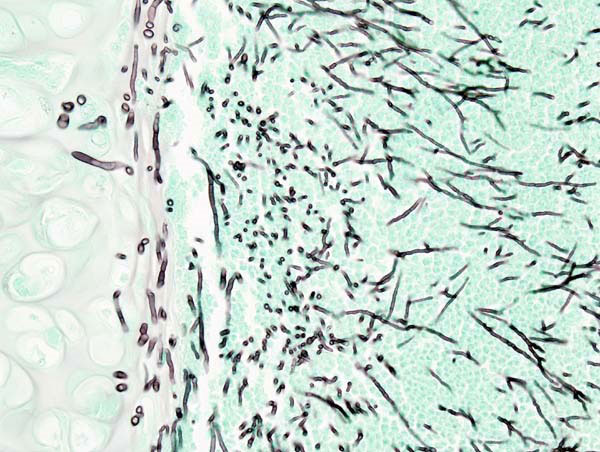
However, even harmless fungi (to healthy individuals) can cause opportunistic infections in an immunocompromised individual. Aspergillosis is one such disease, and it is caused by molds from the genus Aspergillus. There are several forms of this disease, but the most frequent is the mycosis of the lungs (Fig.1). The seriousness of the disease will vary depending on the health of the host, but can often end with a fatal outcome.
Worried About Mold-Related Health Issues? Get a Free Inspection!
Mold like Aspergillus can cause serious health problems, especially for those with weakened immune systems. Don’t let mold go unchecked! Contact Mold Busters for a free virtual mold inspection. Our experts are ready to provide a comprehensive assessment and a plan to tackle any mold issues, ensuring your home is safe and healthy. Act now to protect your health!
What causes Aspergillosis?
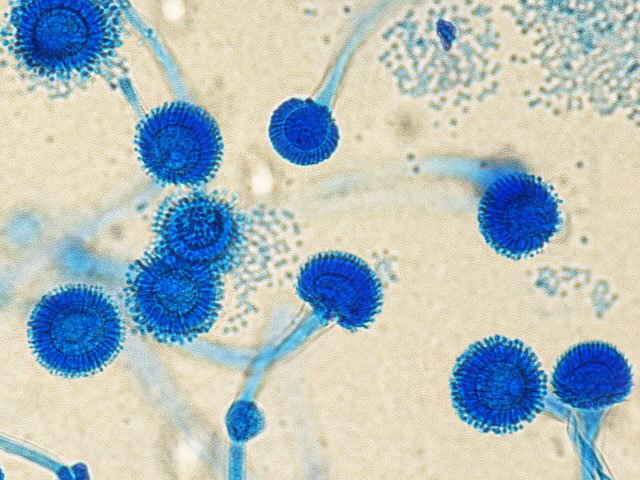
All types of aspergilloses are caused by Aspergillus spp. fungi. This is a diverse genus with high economic and health impacts. Aspergilli (the common name given to these species) are resilient molds, being able to withstand somewhat elevated temperatures and low water availability. They are saprophytic organisms that degrade all types of organic matter. Aspergilli mostly reproduce asexually, they are widespread and can be isolated from all types of surfaces. Of approximately 200 species of Aspergillus, around 20 species are capable of infecting humans and animals (4). Notable mycosis-inducing aspergilli are A. fumigatus, A. flavus, A. terreus, and A. niger (5).
Aspergillus fumigatus is the most common causative species of aspergillosis and can be isolated from most foods and raw materials (Fig. 2). A. fumigatus is a ubiquitous decomposer, often found in substrates rich in organic matter such as soil and compost, where it plays an important role in carbon and nitrogen recycling. For 145 years it was considered to be an exclusively asexual species until the discovery of its sexual stadium – Neosartorya fumigate. Dyer. It can withstand elevated temperatures, which is one of the predispositions for human pathogenicity (as human core body temperature is approximately 37°C (97.9°F). A. fumigatus can grow at temperatures ranging from 12-55°C (53.6-131°F), its spores can survive 70°C (158°F), while its optimum growing temperature is between 40-42°C (104-107.6°F) (6,7).
Aspergillus fumigatus is a mycotoxin-producing fungus, with the foremost, dangerous toxin – Gliotoxin. This is a mycotoxin capable of hindering host defenses through immunosuppression. This toxin attacks white blood cells by inhibiting their migration and offensive enzyme production. It also induces apoptosis (programmed cell death by suicide) in macrophages, white blood cells charged for ingesting and neutralizing foreign elements, and infected cells in the body (8,9).
What are known types of Aspergillosis?
Every day we inhale hundreds of spores of the pathogenic A. fumigatus. In healthy individuals, invading spores are easily recognized by neutrophils (type of white blood cells) and other elements of the immune system and successfully neutralized (7). However, if an individual has neutropenia (low level of neutrophils) or other sorts of immunosuppression due to a disease or a specific medical treatment, spores will germinate and infection will occur. Depending on the location of the infection, and the type of the host’s response, there are several forms of aspergilloses, of which the allergic bronchopulmonary type is the most common (4,10). They are divided into:
- cutaneous aspergillosis
- allergic Aspergillus sinusitis
- allergic bronchopulmonary aspergillosis
- chronic pulmonary aspergillosis
- invasive aspergillosis
Cutaneous aspergillosis
Cutaneous aspergillosis occurs relatively less frequently and usually occurs on parts of skin near catheter or traumatic inoculation sites, sites associated with occlusive dressings, burns, or surgery. It can also form on areas such as the nails, eyes, or ear canals (11).
Allergic Aspergillus sinusitis
Allergic Aspergillus sinusitis is a fungal infection in the sinuses. It causes an immune hyper reaction which results in thick fungal debris, sticky mucus, and blockage of the infected sinuses (12).
Allergic bronchopulmonary aspergillosis
Allergic bronchopulmonary aspergillosis (ABPA) is defined by a hypersensitive response of the host’s immune system to the infecting aspergilli. It is the most frequent in people suffering from asthma or cystic fibrosis, which are bots associated with exacerbated immune system response. Inhalation of the pathogen’s spores causes an improper immune response from the hosts, which results in an allergic reaction to the pathogen. Symptoms usually include wheezing, shortness of breath, and a feeling of general fatigue and poor health, sometimes followed by fever. ABPA may also cause chest pain and bloody coughs. This form of mycosis usually does not metastases (10,13).
Chronic pulmonary aspergillosis
Chronic pulmonary aspergillosis, a condition we frequently encounter during our mold inspections in Montreal, is characterized by the gradual loss of lung tissue and fibrosis (scarring) within the lungs. This usually causes lung cavitation due to the formation of empty spaces, or expansion due to the widening and growth of existing spaces. The thickening of lung membranes may also occur due to this form of aspergillosis (10,13).
A condition often following chronic pulmonary aspergillosis is the formation of a foreign fungal body named aspergilloma. This is a clump of fungal mycelium often mixed in with mucus, tissue debris, inflammatory cells, and fibrin (Fig. 3). Aspergilloma forms in air or cavities within the lungs created during aspergillosis or have been formed from some previous lung disease such as tuberculosis (10).

Invasive aspergillosis
Invasive aspergillosis is a long-term aspergilli infection and it is the most severe form of the disease. It mostly affects individuals who have a severely compromised immune system due to an underlying disease such as certain hematological malignancies (such as leukemia) or AIDS. Invasive aspergillosis also infects individuals receiving chemotherapy, cytotoxic or immunosuppressants therapy due to bone marrow or organ transplants (7).
Invasive aspergillosis usually develops in the lungs and then rapidly travels through the bloodstream (metastases). It is very dangerous as fungal fragments can be carried through the blood system and infect the brain, kidneys, and heart. Infected individuals will often develop fever, headaches, mild hemoptysis (bloody coughs) or sputum, chest pains, and shortness of breath. More severe and life-threatening invasive aspergillosis may cause shock, delirium, massive hemorrhaging from the lungs, and inflammation of the respiratory tract which can cause breathing obstruction. If it has spread to, such as the liver and kidneys, organ failure may occur. If fungal fragments have invaded the central nervous system, the infection may cause seizures, intracranial bleeding, stroke, or meningitis (7,10,13).
How to treat Aspergillosis?
The treatment of aspergillosis, a condition that can be identified through our comprehensive mold testing service in Montreal, will vary depending on the type and levels of the infection, and from the patient’s overall health. In patients with a non-symptomatic aspergilloma, no therapy may be necessary and the individual will be occasionally monitored to detect any developing symptoms. Itraconazole can be administered for individuals who do not have a severe or life-threatening form of aspergillosis.
If the infections are endangering patients’ health, which is why we emphasize on early detection through our mold inspection and testing in Ottawa, the treatment usually involves tested antifungal medications, such as Amphotericin B. These compounds prevent the fungus reproduction and spread, thus giving the body a chance to fight off the infection. Antifungal medications that are also applied against aspergilloses include isavuconazole and voriconazole, and if the patient has not responded to any treatment, caspofungin can be administered. Surgery may have to be conducted to treat certain complications of invasive aspergillosis. However, since this type of aspergillosis occurs in patients with an underlying condition due to a weakened immune system, this solution often comes at a risk (14,15).
References:
- Dressaire, E., Yamada, L., Song, B., & Roper, M. (2016). Mushrooms use convectively created airflows to disperse their spores. Proceedings of the National Academy of Sciences, 113(11), 2833-2838.
- Kadowaki, K., Leschen, R. A., & Beggs, J. R. (2010). Periodicity of spore release from individual Ganoderma fruiting bodies in a natural forest. Australas Mycologist, 29, 17-23.
- Thornton, C. R. (2020). Detection of the ‘Big Five’mold killers of humans: aspergillus, fusarium, lomentospora, scedosporium and mucormycetes. Advances in applied microbiology, 110, 1-61.
- Dagenais, T. R., & Keller, N. P. (2009). Pathogenesis of Aspergillus fumigatus in invasive aspergillosis. Clinical microbiology reviews, 22(3), 447-465.
- Where Aspergillosis Comes From | Aspergillosis | Types of Fungal Diseases | Fungal Diseases | CDC [Internet]. [cited 2021 Oct 22]. Available from: cdc.gov
- O’Gorman, C. M., Fuller, H. T., & Dyer, P. S. (2009). Discovery of a sexual cycle in the opportunistic fungal pathogen Aspergillus fumigatus. Nature, 457(7228), 471-474.
- Latgé, J. P. (1999). Aspergillus fumigatus and aspergillosis. Clinical microbiology reviews, 12(2), 310-350.
- Kamei, K., & Watanabe, A. (2005). Aspergillus mycotoxins and their effect on the host. Medical mycology, 43(Supplement_1), S95-S99.
- Spikes, S., Xu, R., Nguyen, C. K., Chamilos, G., Kontoyiannis, D. P., Jacobson, R. H., … & May, G. S. (2008). Gliotoxin production in Aspergillus fumigatus contributes to host-specific differences in virulence. The Journal of infectious diseases, 197(3), 479-486.https://academic.oup.com/jid/article/197/3/479/2908693
- Aspergillosis – NORD (National Organization for Rare Disorders) [Internet]. [cited 2021 Oct 22]. Available from: rarediseases.org
- Van Burik, J. A. H., Colven, R., & Spach, D. H. (1998). Cutaneous aspergillosis. Journal of clinical microbiology, 36(11), 3115-3121.
- Dolen, W. K. (2006). Risk factors for allergic Aspergillus sinusitis. Medical mycology, 44(Supplement_1), S273-S275.
- Kousha, M., Tadi, R., & Soubani, A. O. (2011). Pulmonary aspergillosis: a clinical review. European Respiratory Review, 20(121), 156-174.
- Walsh, T. J., Anaissie, E. J., Denning, D. W., Herbrecht, R., Kontoyiannis, D. P., Marr, K. A., … & Patterson, T. F. (2008). Treatment of aspergillosis: clinical practice guidelines of the Infectious Diseases Society of America. Clinical infectious diseases, 46(3), 327-360.
- Treatment for Aspergillosis | Aspergillosis | Types of Fungal Diseases | Fungal Diseases | CDC [Internet]. [cited 2021 Oct 23]. Available from: cdc.gov
Get Special Gift: Industry-Standard Mold Removal Guidelines
Download the industry-standard guidelines that Mold Busters use in their own mold removal services, including news, tips and special offers:
Published: October 28, 2021 Updated: July 1, 2024

Written by:
Dusan Sadikovic
Mycologist - MSc, PhD
Mold Busters
Fact checked by:
Michael Golubev
CEO
Mold Busters
