Fresen. 1850
What is Mucor mucedo?
Mucor mucedo, commonly known as the common pinmold, is a ubiquitous fungal saprophyte and a pathogen. M. mucedo belongs to the family Mucoraceae, ordo Mucorales. These species are associated with now polyphyletic (share common characteristics but do not have a common ancestor), but ancient group (phylum) of fungi, Zygomycetes. Members of this group of fungi represent one of the most primitive fungal forms, which has diverged very early from the dominant, higher fungi such as Ascomycota and Basidiomycota (1,2).
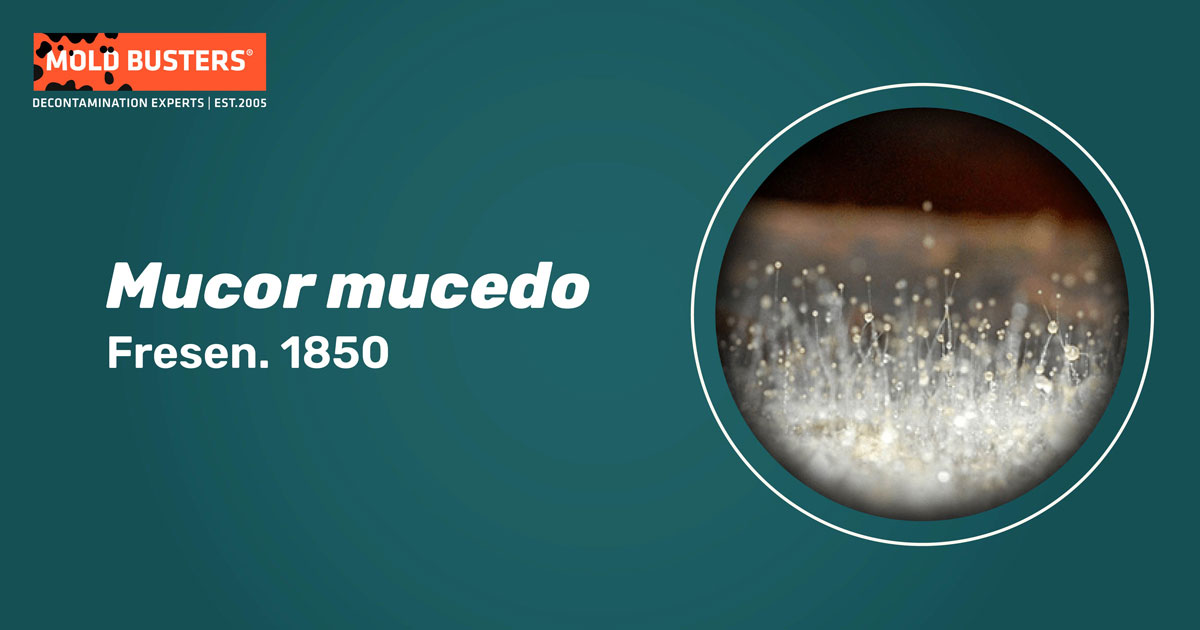
Mucor mucedo and, generally, other Mucorales are usually first saprophytic colonizers on dead or decaying organic material (Fig. 1). They can rapidly utilize the limited amounts of simple carbohydrate molecules available before other fungal competitors. All Mucorales are generally fast-growing fungi – in cultures and nature. Especially those competitors that can feed on complex carbohydrates such as lignin, and dominate the decomposition process (3).

Mucor mucedo ecology
Being present on most continents (apart from Antarctica), M. mucedo has a worldwide distribution. In nature, it can be commonly found in soil and animal dung, especially during springtime. M. mucedo can also be frequently found contaminating stored grain, and fruits and vegetables such as grapes and tomatoes. This fungus can cause cheese spoilage, thereby giving the cheese cat a hair-like appearance, due to the development of grayish long sporangiophores (Fig. 2). M. mucedo can also act as an animal pathogen, infecting horses, rabbits, mice, and rats. Indoors, Mucor mucedo spores can be found in household dust, carpets, mattresses, ventilation ducts, and can grow on water-damaged structural material (4,5).

What does Mucor mucedo look like?
Mucor mucedo colonies commonly display a fluffy appearance with sporangia reaching heights of up to several centimeters, which gives the colony the resemblance to cotton candy. The hyphae are non-septate or sparsely septate. Although Mucorales reproduce sexually by the formation of zygospores, traditional classification has been based on asexual reproduction. Sporangiospores, formed in asexual production, are typically borne within sporangia. These structures are terminally-formed closed sacs on elongated stalks (stipes) (Fig. 3). M. mucedo has unbranched sporangia, without basal rhizoids. Zygosporangia, formed in sexual reproduction, have pigmented walls, covered with granules. The growth of M. mucedo colonies is influenced by light. Cultures cultivated during the day at 20 °C (68°F) produce mostly tall sporangiophores, while those grown in the dark produce a thick layer of short sporangiophores, with tall ones occasionally protruding (3,5).

Mucor mucedo toxicity
Mucor mucedo produces a mycotoxin oxalic acid. This is well known to be toxic to higher organisms, including humans, due to its local corrosive effect and affinity for calcium ions. One of the known effects of this acid is the formation of large kidney stones, because oxalic acid combines with positively charged ions such as calcium (Ca2+), thus forming water-insoluble calcium crystals which cause infections, pain, and discomfort, especially when excreted through urine (6).
Mucor mucedo as human pathogen
In rare cases, Mucor mucedo can cause fungal infections known as mucormycosis. Healthy humans can normally fight Mucor spp. spores with ease, as our immune systems have evolved the handle hundreds of different fungal spores that we inhale daily. However, in immunocompromised individuals, mucormycosis can be extremely dangerous and often ends with high mortality rates.
Mucor spp. infections are characterized by fungal vascular invasion, leading to thrombosis, infarction, and necrosis of the infected tissue because the fungal mycelium feeds on the dead organic matter (7). Mucor infections usually occur through the inhalation of spores, but they can also be achieved by ingestion and through surgical and accidental wounds. Mucorales fungi are attacked blood vessels (vasculotropic fungi), and therefore hyphal infiltrations can often occur in the vicinity of blood vessels of the primary infected organs (8,9).
Healthy humans are usually not at risk and common underlying diseases are connected with Mucor spp. infections include blood diabetes (with or without diabetic ketoacidosis), blood malignancies such as leukemia, as well as solid organ tumors. Patients undergoing corticosteroid therapy due to organ or bone marrow transplants are especially at risk because this therapy significantly suppresses their immune system (10).
Did you know?
Bathrooms in Canada are the most affected by the Basidiospores mold group?! Find out more exciting mold stats and facts inside our mold statistics page.
References
- Morin-Sardin, S., Nodet, P., Coton, E., & Jany, J. L. (2017). Mucor: A Janus-faced fungal genus with human health impact and industrial applications. Fungal Biology Reviews, 31(1), 12-32.
- Krings, M., Taylor, T. N., & Dotzler, N. (2013). Fossil evidence of the zygomycetous fungi. Persoonia: Molecular Phylogeny and Evolution of Fungi, 30, 1.
- Robinson, R. K. (2014). Encyclopedia of food microbiology. Academic press.
- Stern, A. M. (1951). Studies on the Physiology of the Mucor Mucedo and Its Role in the Fermentation of Soybean Curd. University of Illinois at Urbana-Champaign.
- Pitt, J. I., & Hocking, A. D. (2009). Fungi and food spoilage(Vol. 519, p. 388). New York: Springer.
- Kadis, S., Ciegler, A., & Ajl, S. J. (1971). Microbial toxins. Vol. VII. Algal and fungal toxins. Microbial toxins. Vol. VII. Algal and fungal toxins.
- Chowdhary, A., Perfect, J., & de Hoog, G. S. (2015). Black molds and melanized yeasts pathogenic to humans. Cold Spring Harbor perspectives in medicine, 5(8), a019570.
- Eucker, J., Sezer, O., Graf, B., & Possinger, K. (2001). Mucormycoses. Mycoses, 44(7‐8), 253-260.
- Pagano, L., Ricci, P., Tonso, A., Nosari, A., Cudillo, L., Montillo, M., … & GIMEMA Infection Program. (1997). Mucormycosis in patients with haematological malignancies: a retrospective clinical study of 37 cases. British journal of haematology, 99(2), 331-336.
- Skiada, A., Pagano, L. I. V. I. O., Groll, A., Zimmerli, S., Dupont, B., Lagrou, K., … & Petrikkos, G. (2011). Zygomycosis in Europe: analysis of 230 cases accrued by the registry of the European Confederation of Medical Mycology (ECMM) Working Group on Zygomycosis between 2005 and 2007. Clinical Microbiology and Infection, 17(12), 1859-1867.
Get Special Gift: Industry-Standard Mold Removal Guidelines
Download the industry-standard guidelines that Mold Busters use in their own mold removal services, including news, tips and special offers:

Written by:
Dusan Sadikovic
Mycologist – MSc, PhD
Mold Busters
Fact checked by:
Michael Golubev
General Manager
Mold Busters
